As health care providers observe Coronavirus Disease 2019 (COVID-19) affecting children differently than adults, pediatric surgeons in Chicago have modified an evaluation tool for use in pediatric patients that allows surgeons in every pediatric specialty to prioritize nonemergency (“elective”) operations during all phases of the pandemic. The new pediatric-specific scoring system is presented in an “article in press” on the Journal of the American College of Surgeons (JACS) website ahead of print.
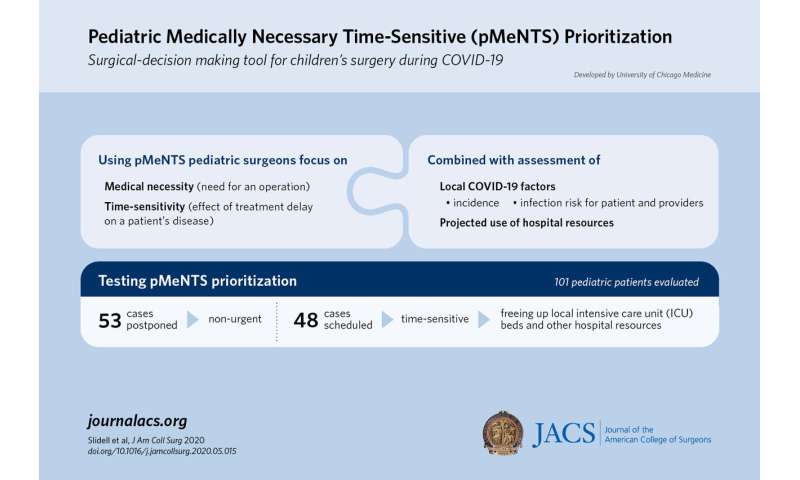
Called the Pediatric Medically Necessary Time-Sensitive, or pMeNTS, scoring system, the new index score created by researchers at The University of Chicago (UChicago) Medicine adapts the adult MeNTS approach. That original surgical prioritization approach was published on April 9 in a scientific article on the JACS website amid COVID-19-related resource constraints and nationwide recommendations to postpone elective operations.1
Pediatric surgeons at UChicago Medicine found that the adult MeNTS scoring system needed revisions for optimal use in pediatric surgery, according to Mark B. Slidell, MD, MPH, FACS, the lead investigator and associate professor of surgery at UChicago Medicine.
“It was very important to create a pediatric-specific system that recognizes there are big differences between adults and children,” Dr. Slidell said.
Need for revised scoring system
Among the differences is that many children testing positive for COVID-19 appear asymptomatic (have no symptoms).2 Also, recent reports noted a new serious complication of COVID-19 in some infected children, including those who were unaware they had the virus: an inflammatory syndrome that can lead to severe involvement of multiple organs.2
Dr. Slidell’s coauthor, Grace Z. Mak, MD, FACS, UChicago Medicine associate professor of pediatrics and surgery, said users of the pMeNTS scoring worksheet can adapt it to include new COVID-19 developments.
“Part of what we took into account is that asymptomatic COVID-positive patients in the pediatric population could very well have a worse outcome, and multisystem organ failure is a good example,” Dr. Mak said.
As the pandemic changes the concept of elective operations, pMeNTS focuses on an operation’s medical necessity and time-sensitivity—the effect of treatment delay on the patient’s disease. Plus, it assesses COVID-19 factors such as infection risk for the patient and providers as well as projected use of hospital resources, including protective gear, beds, blood products, and staffing. The tool, which Dr. Slidell emphasizes is not a risk calculator, systematically evaluates factors related to the procedure, the patient’s disease, and the patient’s individual risks. Users rate each factor on a five-point scale and total the scores. A lower overall pMeNTS score indicates a more favorable surgical risk, less risk to personnel, and less resource utilization, and can be used to determine a higher priority for the procedure.
The hospital’s surgical department leaders review the assigned scores for each surgical case and can shift the scoring cutoff each day for high-priority operations depending on available resources, Dr. Mak stated.
Unlike the adult scoring system, pMeNTS accounts for chronic diseases of childhood and birth defects such as prematurity or congenital heart and lung diseases that may raise susceptibility to more severe COVID-19 infection. It omits chronic illnesses of adulthood that are rare in children such as coronary artery disease and chronic obstructive pulmonary disease.
Another key change was pediatric age brackets reflecting the impact of age on a procedure. For instance, Dr. Mak said a hernia repair is a more difficult operation in a premature infant than a 14-year-old patient. In the adult MeNTS system, both patients would have the same score, but pMeNTS accounts for the child’s age and assigns the infant a higher number, she explained.
Testing the system
The investigators tested pMeNTS in 101 pediatric patients scheduled for operations at UChicago Comer Children’s Hospital from March 23 to April 19. In the article, they reported the system to be “a safe, equitable, transparent, and ethical strategy to prioritize children’s surgical procedures.”
During that month, they analyzed a sample of 53 deferred cases and 48 cases that were allowed to proceed as scheduled. Procedures they deemed time-sensitive included cancer biopsies and operations needed for discharge from the intensive care unit (ICU), thus freeing ICU beds, Dr. Mak said.
The researchers also compared scores of a sample of 21 patients using both the pediatric and adult scoring systems. Most children, they found, had higher scores with the adult MeNTS. Dr. Slidell said pMeNTS successfully captured the various factors that are unique to children.
Strengths of the pMeNTS tool, according to Dr. Slidell, include the flexibility to adapt to changes in the health care system now and during recovery from the pandemic. Because the tool received input from many different specialists, he said it works well across various pediatric surgical subspecialties.
Source: Read Full Article


