A Vanderbilt cancer systems biology team has identified the enzymes that keep tumor cells growing in the presence of drug treatment, opening the door to stopping these cells dead in their tracks.
An article, “An Integrative Gene Expression and Mathematical Flux-Balance Analysis Identifies Targetable Redox Vulnerabilities in Melanoma Cells,” was published in the journal Cancer Research on Oct. 15.
Until about 10 years ago, the cancer research community mainly concentrated on cancer cell mutations and how to shut them down. This focus paid off in the form of treatments that could essentially turn off a gene that appears in about half of all skin cancers to mutate and regulate tumor cell growth. Unfortunately this costly and grueling therapy had its limits. Tumors in only half of patients would disappear for anywhere from a month to a year, and then the cells that survived–unaffectionately known as drug-tolerant persister cells–would return.
“We set out to explore, on the single tumor-cell level, the perplexing question of why some tumors are wiped out when they’re hit with BRAF inhibitors and why others are not,” said Vito Quaranta, professor of biochemistry and pharmacology. “We combined our studies of gene expression and metabolomics with a data science approach to identify the clear source of the differences that, beyond genetics, make some cells vulnerable to BRAF inhibitors and others not.”
In discerning how persister cells survive through cancer treatment and continue to grow, Quaranta’s team–Quaranta Lab postdoctoral fellow Bishal Paudel, Stevenson Professor of Chemistry and chair of the Department of Chemistry John McLean, and Georgia Tech bioengineering professor Melissa Kemp–examined baseline metabolic features that “prime” melanoma cells to become drug-tolerant persisters.
“Our approach is a departure from a genetics-centered view in cancer treatment, and we hope the field will appreciate that cancer treatments need to be dynamic, as tumors often change their phenotypes,” said Paudel, the paper’s first author.
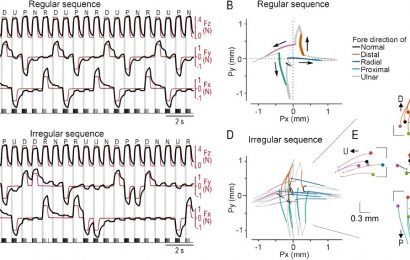
The collaborators hypothesized that the logical place to look for differences was the nutrients and energy that the cells receive during and after the BRAF gene is inhibited. Using metabolomics–the measurement of certain substances necessary for metabolism–and machine learning to classify cells, the team found the source of energy for drug-tolerant cells is centered around redox balance and NOX5, an enzyme that is elevated in melanomas resistant to treatment.
“The drug-tolerant cell’s reliance on NOX5 and redox balance for energy is akin to people turning on a generator during a power outage,” said Quaranta, who also is director of the Vanderbilt University Quantitative Systems Biology Center. “The enzyme also produces waste, like fumes emitted from a generator, that enhanced antioxidant capabilities supported by the cysteine transporter SLC7A11 help rid the cell of. Now that we understand this mechanism, the enzyme’s vulnerabilities and a delicate pathway balance, we are set up to take them down.”
“Working with single cell gene expression patterns, our group leveraged machine learning techniques to broadly understand how metabolism is wired in different cell types, and to predict that certain substances necessary for metabolism in persister cells were higher than drug-sensitive cells,” said Kemp, a Georgia Cancer Coalition Distinguished Cancer Scholar. “Using normal skin cells as a baseline and data provided by the Quaranta Lab, we can now classify cells as drug-tolerant and -sensitive, making it much more effective to study persister cells and the best way to finish them off for good.”
“Metabolomics has grown as a research field within the last decade and applying it to this research has resulted in highly impactful conclusions,” McLean said. “The difficult-to-produce data that has identified NOX5 and redox balance as the key players in a melanoma’s survival is going to change the way that the entire cancer research community thinks about curing cancer.”
While NOX5 is not present in all tumors, this redox balance framework of drug-tolerant cells may be consistent across other cancer types. The team’s next step, as it relates specifically to melanoma research, is to find the most effective tactic to go after NOX5–either by finding a way to destroy the enzyme itself or a way to inhibit the antioxidant ability of the cell. For other cancer researchers, these findings are key to helping identify enzymes that enable other cancers’ drug-tolerant persister cells in hopes of exploiting their vulnerabilities.
Source: Read Full Article